Crosby Health
About Crosby Health
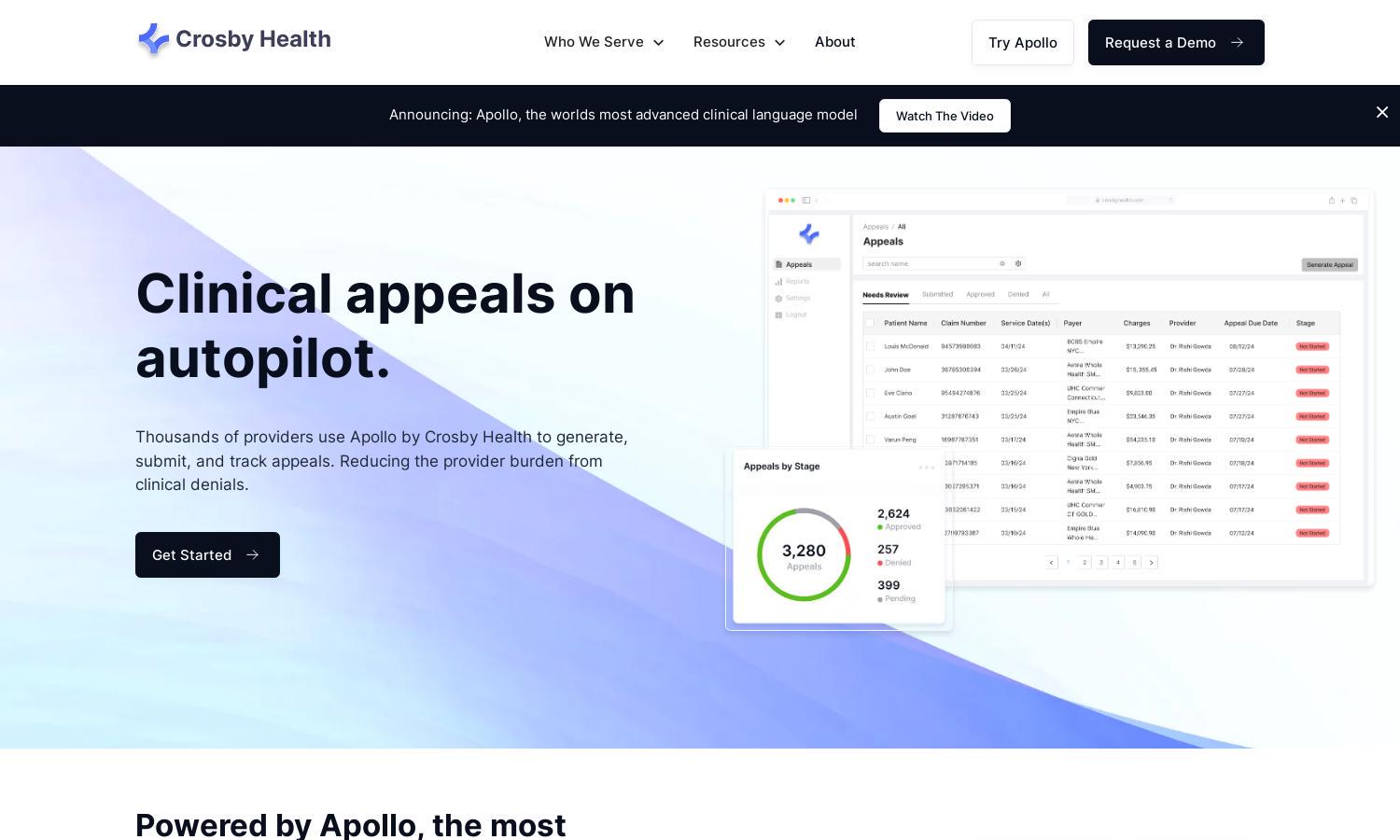
Crosby Health provides a revolutionary platform for healthcare providers to automate clinical appeals. Utilizing Apollo, the most advanced clinical AI, users can effortlessly generate, submit, and track appeals. This innovative service reduces administrative burden and enhances recovery rates, making it an essential tool for hospitals and practices.
Crosby Health offers various pricing plans tailored to different needs, ensuring accessibility for all providers. Each subscription tier delivers robust features, helping users maximize their claim recovery. Upgrading grants access to advanced automation benefits, enhancing efficiency and streamlining appeals management for higher performance.
Crosby Health's user interface is designed for simplicity and efficiency. Its intuitive layout enables seamless navigation, allowing users to quickly access features like appeal generation and tracking. User-friendly elements, such as one-click submissions and automated notifications, enhance the overall experience on the platform.
How Crosby Health works
To interact with Crosby Health, users start with a simple onboarding process where they input necessary information. After onboarding, they can navigate the platform to generate appeal letters using AI, submit them to payors with one click, and track each appeal’s progress. The integration of legal and clinical guidelines ensures accurate submissions, reducing denials and enhancing recovery.
Key Features for Crosby Health
Automated Appeal Generation
Crosby Health features automated appeal generation, allowing users to create detailed and compelling appeal letters with minimal effort. This streamlined process maximizes recovery on claim denials, significantly reducing administrative workload for healthcare providers and enhancing overall efficiency.
Integrated Payor Submission
Crosby Health offers integrated payor submission, simplifying the appeals process by allowing one-click submission to multiple insurance companies. This feature consolidates the cumbersome task of managing numerous payor portals, making it easier for providers to handle claim denials efficiently.
Real-Time Tracking and Notifications
Crosby Health includes real-time tracking and notifications for each appeal submitted. Users receive immediate alerts regarding the status of their appeals, ensuring they stay informed and can respond promptly to payor decisions, ultimately improving recovery timelines and outcomes.
You may also like:








